Why Is Catheterization Knowledge So Important?1-7
Urologists report an increasing volume of urology referrals and consults with catheterization making up a significant portion of those consults. Additionally, there appears to be an increase in the number of iatrogenic UC trauma cases. While one may assume that junior staff are responsible for this increase, recent studies have found an increasing number are caused by experienced healthcare staff who were routinely involved in catheterization.
Improper UC can lead to urethral complications and mild or serious injury and lead to long term sequalae including strictures, incontinence infertility and erectile dysfunction. It has been reported that ~40% of urethral strictures are caused by urethral trauma and makes future catheterizations more difficult and may require more advanced invasive procedures to repair.
One US study in a large tertiary-care hospital over a 1-year period reported that of 613 urology consults, 319 (52%) were potentially unnecessary consults resulting in a loss of 265.8 hours for urologists and incremental $44,376.09 in health care costs.6
Several studies of the knowledge, skills and confidence among healthcare workers in hospitals concerning urinary catheterization have been done. The results of such studies have clearly indicated there is a lack of adequate training and confidence in urinary catheterization from medical interns, residents, and nurses and a need to refresh these skills even in experienced physicians and nurses.1,3
With about 25% of hospital inpatients being catheterized at any one time and the regular appearance of patients coming into the Emergency Department requiring urinary catheterization (UC), the need for catheterization knowledge and skills has never been greater.
Knowledge and Attitudes and Skills of Healthcare Practitioners
in Urinary Catheterization1-7
Most urethral catheter placements are performed initially by a nurse or resident.
One study reported that in >50% of catheter referrals no attempt at urinary catheterization is made, then a urologist performs the procedure with no issue or special adjuncts. In one hospital, up to 70% of consults for catheterization lead to delays in patient care, and added unnecessary complexity to patient care and increased total healthcare costs.
- A 2013 study by Bacsu on difficult UC, found a delay in consult from the 1st time a catheter was attempted had a mean wait time of 262 minutes, and a range of 0-3 days noting that this delay can cause significant anxiety, discomfort, and risk for severe complications in patients.
- One Irish study reported 76% of interns felt their practical UC training nearly non-existent and 52% performed their first UC without supervision
- A 6-month audit of a hospital on Iatrogenic UC was performed, then an educational workshop available for all staff, then a follow up 6 month audit:
- The pre-education rate of iatrogenic UC was 4.3/1,000 catheters compared to 3.8/1,000 catheters post-education
- In the 12-month audited period, 25 iatrogenic UCs occurred, and all 25 were done by doctors experienced with UC
- While fewer iatrogenic UC occurred post education, the data suggest the need for reinforcement of correct technique and knowledge be conducted routinely even for all regular performers of UC.
- A study with medical students in 2nd and 3rd year found low levels of confidence in all skills of catheterization, knowledge, troubleshooting and placing a catheter in the same or opposite gender.
- Immediately following a didactic training session taught by senior urology residents and use of simulators; confidence levels increased significantly, and this effect was sustained and increased slightly 3-6 months later, with 83% of them feeling fully trained.
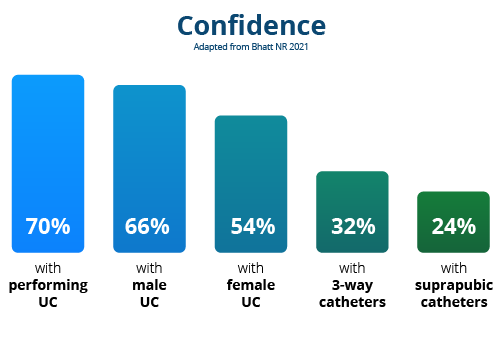
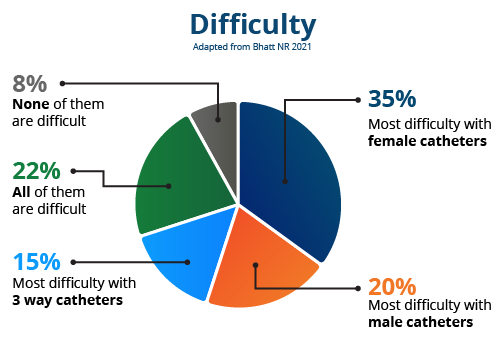
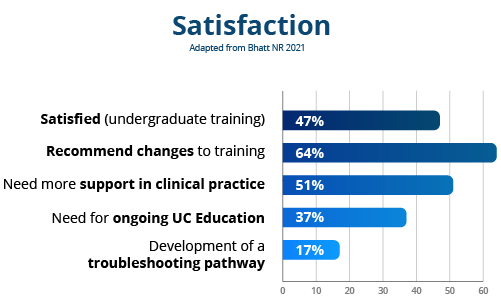
- In 2021 a hospital study by Bhatt was undertaken to determine the confidence and knowledge of UC across specialties and grades:
- 90 respondents: Medicine 39%, Surgery 26%, Community 13%, Emergency 8%, Obstetrics & Gynecology 7%, Anesthesiology 5%, Pediatrics 2% Respondents had a median of 4 years clinical experience (1-40 years experience)
- 57% had no previous urological experience
- Of the 90 respondents, over 50 dealt with UC at least weekly
- 93% of respondents were involved in catheterizing patients as part of their role
- 60% incorrectly identified catheter types from options
- 90% of respondents felt formal UC training should be compulsory
From this study and others like it the evidence points to a need to improve catheter training not only in the undergraduate setting but as part of a routine standardized program for all staff members who may be required to insert a catheter.
There is a need:
- For understanding different catheters and their application and in understanding the complexities and how to manage difficult catheterizations.
- To ensure that sufficient time is spent on both male and female catheterizations.
Teaching should be done by highly experienced staff members from urology with both a didactic session and workshops with the use of catheterization simulation models if possible.
Training should be done in all departments with particular focus on those departments such as the Emergency Department which catheterizes patients with very limited urologic knowledge of that patient.
Active involvement of the urology department in initiating regular catheter refresher training is a key factor in creating a successful training program.1-7
The results of a urinary catheter educational program are:
- Increased staff confidence and skill in urinary catheterization
- Reduced wait times for patients, with less unnecessary procedures
- A reduction in the number calls for urology consults, particularly outside of regular working hours
- A reduction in the number of iatrogenic injuries and trauma
- A reduction in the number of surgical interventions to repair iatrogenic injury
- A savings in urology hours for unnecessary consults and a cost savings to the healthcare system
Why Not Set Up A Catheterization Training Program in Your hospital? Biosyent Can Help.
BioSyent recognizes the value of catheterization education and has undertaken initiatives to support hospitals in their desire to improve their staff’s knowledge and understanding of catheterization.
- BioSyent offer some financial support to help in preparing and running training events or to fund speakers to provide the training.
- BioSyent also has some presentations that staff can adapt to help them with setting up their own training presentation.
- Speakers from the Urology Nurses of Canada who can present on a variety of catheterization related topics and provide firsthand information on managing difficult urinary catheterizations in a variety of patient scenarios.
For more information on how BioSyent can help you set up a catheterization training event in your hospital, simply fill in the contact information on the contact page or reach out to your BioSyent Specialist Representative if you have their contact information. We will get back to you quickly to help with your catheterization educational program.
References
- Bhatt NR, Davis NF, Thorman H, et al. Knowledge, skills, and confidence among healthcare staff in urinary catheterization. Can Urol Assoc J 2021;15(9):E488-94. http://dx.doi. org/10.5489/cuaj.6986
- Cohen et al, Attitudes and knowledge of urethral catheters: A targeted educational intervention, BJU Int 2016; 118: 654–659, doi:10.1111/bju.13506
- Bhatt NR et al, A prospective audit on the effect of training and educational workshops on the incidence of urethral catheterization injuries, Cite as: Can Urol Assoc J 2017;11(7):E302-6. http://dx.doi.org/10.5489/cuaj.4271
- Manalo. et al, Medical interns’ knowledge and training regarding urethral catheter insertion and insertion-related urethral injury in male patients, BMC Medical Education 2011, 11:73, http://www.biomedcentral.com/1472-6920/11/73
- McDermott, Patricia; Teaching patients self-catheterisation in an emergency department, Nursing Times [online] June 2020 / Vol 116 Issue 6 p32-35
- Hanson Z et al, Characteristics, Burden, and Necessity Inpatient Consults for Academic and Private Practice, Urology Health Services Research, Volume 139, P60-63, May 01, 2020, 2020DOI:https://doi.org/10.1016/j.urology.2020.02.016
- Bacsu, Chasta et al, A prospective analysis of consultation for difficult urinary catheter insertion at tertiary care centres in Northern Alberta, CUAJ Sept-Oct 2013 Vol 7, issues 9-10


 2476 Argentia Road, Suite 402
2476 Argentia Road, Suite 402 1.888.439.0013
1.888.439.0013 905.206.1413
905.206.1413 cathejell@biosyent.com
cathejell@biosyent.com