Tips & Tricks
Female Urethral Catheter Instillation
General Tips
- Set expectations with the patient so they know what to expect, tell them firm genital contact is needed. This should relieve some anxiety and possible pelvic tension)
- Ensure good lighting or use a flashlight/headlamp
- Utilize a second pair of hands when needed
- Tilt the patient’s pelvis up by using a folded towel under the lower back or a pillow under the buttocks
- Elevating the pelvis when possible allows you to insert the catheter in a downward motion rather than the elusive upward motion (which is where the meatus ends up and insertion is mostly blind), making it less likely to place the catheter mistakably into the vagina
- If you miss the urethra and put the catheter into the vagina, leave it there as a marker, then get a fresh catheter and aim for the higher opening. Once you’ve got the catheter in the bladder, remove the unneeded catheter from the vagina
Finding the Urethra6
Sometimes the urethra in women can be difficult to find as in the case of atrophic vaginitis when the urethral meatus has retracted into the vaginal opening. As you spread the labia you may not see the urethral meatus, but by placing your finger at the anterior surface of the vagina you can feel the meatus and it will feel like a buttonhole. Now you can use your finger to carefully guide your catheter into the urethra and into the bladder.
Sometimes the urethral meatus can be found by inserting a Coudé tip catheter with the tip facing up along the anterior surface of the vagina where it will encounter and slip into the urethral meatus.
Cleanse or Cough
- With your dominant hand, using forceps and betadine-soaked cotton swabs or soap and water, cleanse the meatus and watch for the “wink” (the urethral opening will slightly open and appear to wink at you)
- Having the patient cough will also cause the urethral “wink”
Challenging Patients to Catheterize
Obese Women
 Side-Lying Position
Side-Lying Position
- Flex hips and knees and elevate top leg and the upper leg held by a helper
- Improves view
- Improves access to the urethral meatus
- Don’t be afraid of moving the tissues around until you find urethra
- On larger women, the labia also gets fat and the meatus can be much deeper

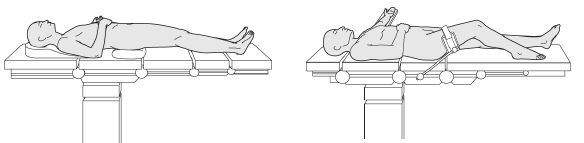
Trendelenburg Position
- Flat on back with feet 15⁰–30⁰ higher than head
- For obese female patients, the abdominal pannus or “apron”, falls back (towards her head) and out of the way
- Utilize another nurse to hold/spread the patient’s legs and labia further apart
- If you put a little extra pressure when cleaning it may cause the meatus to react, like a wink, and be visible
- If still not visible, use of a vaginal speculum and surgical spotlight can help
- Place a finger into the vagina a few cm below the clitoris, push in and up and this may help expose the urethral meatus. Then wipe the area with betadine to cause the meatus to “wink” so the opening can be seen.
- Alternatively you could ask the patient to cough which may also cause a reaction in the meatus
Elderly Women
 Legs Up and Back
Legs Up and Back
- Ideal for older women who have difficulty opening their legs
- Lifting/holding the patient’s legs straight up and back a bit (or use stirrups) for improved visualization and access to the urethral meatus
- Use the bottom half of a plastic speculum (lubricate and place into the vagina) to hold the labia out of the way and to see the urethral meatus much better
- You can also put the patient in the Trendelenburg position
- Use a helper if she can’t hold her legs very far apart
- If the patient has atrophic vaginitis, placing your finger at the anterior surface of the vagina you can feel the meatus and it will feel like a buttonhole. Now you can use your finger to carefully guide your catheter into the urethra and into the bladder
Supine Position
- Knees flexed and separated; feet flat on bed about 60 cm apart
- If uncomfortable, instruct patient to either flex one knee (with other leg flat on the bed), or spread her legs as far apart as possible
- Use the back side of your hand and gently push the labia majora up to make the urethra more visible
- Separate the labia majora and labia minora with thumb, middle, and index fingers of your non-dominant hand, and push up slightly (puts tension on the tissue, helping to stabilize the position of the meatus)
- Push up slightly causing the meatus to be visible and puts a little tension on the tissue stabilizing the position of the meatus
- If you don’t have extra hands, you can, use sterile 4×4 Band-Aids to hold the labia open so you can see and access it
Click here for Tips & Tricks on Male Urethral Catheter Instillation
References for Tips & Tricks
- Carlos Villanueva, George P. Hemstreet III, Difficult Male Urethral Catheterization: A Review of Different Approaches, International Braz J Urol, Vol 34 (4):401;412, July-August, 2008, https://www.scielo.br/j/ibju/a/n6MzhTpdSCWHpJTvc7JWMbb/
- Bacsu, Chasta et al, A prospective analysis of consultation for difficult urinary catheter insertion at tertiary care centres in Northern Alberta, CUAJ Sept-Oct 2013 Vol 7, issues 9-10, https://cuaj.ca/index.php/journal/article/view/574
- Paul Willette and Scott Coffield, Current Trends in the Management of Difficult Urinary Catheterizations, Western J of Emergency Medicine, vol XIII, no 6 Dec 2012 p 472-478 doi: 10.5811/westjem.2011.11.6810 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3555603/
- Mario Gardi et al, The Challenge of Difficult Catheterization in Men: A Novel Technique and Review of the Literature, UroToday Int J. 2013 August;6(4):art 53. http://dx.doi.org/10.3834/uij.1944-5784.2013.08.12
- Leon-Mata et al. Tips and Tricks for Difficult Urethral Catheterization. International Annals of Medicine. 2018;2(1). https://doi.org/10.24087/IAM.2018.2.1.396
- Cameron Ghaffary, et al, A Practical Approach to Difficult Urinary Catherizations, Curr Urol Rep (2013) 12:565-579 DOI 10.1007/s11934-013-0364-3
- Alexa Bianchi; Stephen W. Leslie; Gregory T. Chesnut., Difficult Foley Catheterization, Oct 5, 2022, https://www.ncbi.nlm.nih.gov/books/NBK564404/


 2476 Argentia Road, Suite 402
2476 Argentia Road, Suite 402 1.888.439.0013
1.888.439.0013 905.206.1413
905.206.1413 cathejell@biosyent.com
cathejell@biosyent.com